Urethral Stricture
Abnormal narrowing of the urethral lumen, mainly due to fibrosis of the inner skin of urethra causing difficulty for the passage of urine is called Urethral stricture. Sometimes the flow of urine is completely stopped resulting in complete retention of urine.
Urethral stricture is a disease of sexually active age group (i.e. between 16 and 60 years) and is more common in males than females.


Anatomy
Language: Hindi
Language: English
Male Urethra
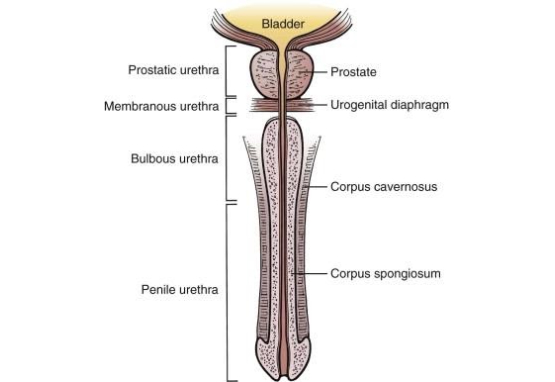
- Extends from Bladder neck up to Meatal opening over Glance Penis
- About 20cm in length and runs through the Corpus Spongiosum
- Divided as Anterior Urethra and Posterior Urethra by Pelvic Diaphragm
- Anterior Urethra consists of Bulbar and Penile parts of Urethra
- Posterior Urethra consists of Membranous and Prostatic parts of Urethra
- Normal Diameter of Urethra is about 6mm
Female Urethra

- Extends from Bladder neck up to the external opening in the vestibule
- About 4cm in length
- Normal Diameter of Urethra is about 6mm
Physiology
Language: Hindi
Language: English

- The urethra is a collapsible pipe which usually remains closed for all the time and opens when a person urinates
- Urethra being a collapsible pipe doesn’t have its diameter
- Being a collapsible pipe urethra has its two distinct properties –
- Elasticity – By which it can open and close
- Caliber – The maximum extent to which it can open
Pathology
Language: Hindi
Language: English

Pathology of urethral stricture starts with ulceration or wound inside the urethra. Whenever there is a wound on any surface of our body, that wound eventually heals. When it heals, it leaves a scar. The scar left is much smaller as compared to the actual size of the wound. This is called as wound contraction or cicatrization of the wound. So any wound, when it heals it contracts significantly and this contraction is by almost 40 to 80%.
When there is a wound or ulceration inside the urethra that also contracts significantly. Urethra being a very small pipe when the wound contact at the same time the whole pipe of urethra gets constricted significantly and thus the lumen becomes narrow.
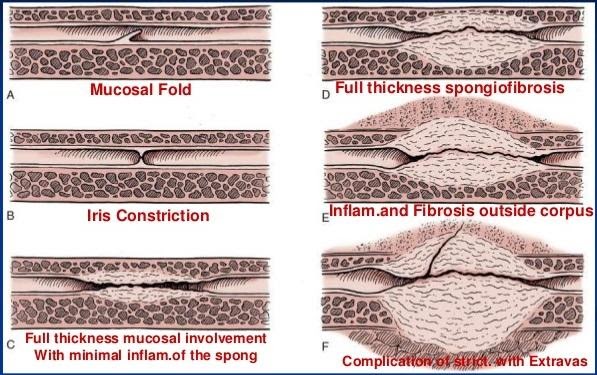
A wound heals by granulation. Even in case of deeper wounds, the granulation starts from the base of the wound and when that granulation reaches up to the normal level of the skin or epithelium, the process of granulation stops at that level. Generally, the granulation never overgrows the normal level of the skin or epithelium.
The urethra is a pipe through which urine passes many times a day. Urine is acidic & it contains many salts, so it interferes with the normal healing process. Healing being a natural process, nature tries her best to heal that wound at any cost, and in that attempt, the rate of granulation significantly increases. Thus, the process of graduation, which should stop at the normal level, there is little overgrowth inside the lumen of the urethra. This overgrown tissue is called as over granulation or hyper granulation. This results in further narrowing of the lumen. Initially, the hyper granulation is soft but later it turns into fibrosis and it becomes hard. This is also called the actual scar tissue of the stricture, which results in loss of distinct qualities of urethra i.e. elasticity & caliber at that particular point.
Causes
Language: Hindi
Language: English




Symptoms
Language: Hindi
Language: English
Storage LUTS

- Frequency
- Urgency
- Nocturia
- Urge incontinence
- Stress incontinence
- Incontinence
- Enuresis
- Pelvic pain
Voiding LUTS

- Incomplete emptying
- Episodes of near retention
- Voiding small volume
- Spraying / double stream
- Haematuria
- Burning & Dysuria
- Straining
- Hesitancy
- Poor flow
- Dribbling
- Intermittency
Additional LUTS

- Haemospermia
- Retrograde ejaculation
- Discharge from urethra
- Reduced ejaculation force
- Pain in scrotum / testicles
- Dyspareunia
- Fever with chills & rigors
Diagnosis
Language: Hindi
Language: English
1. Proper History taking
2. Clinical Examination
3. Uroflowmetry
- The investigation is done to know the exact flow rate of urine during micturition
- Maximum flow rate (Q max) – Should be at least 15ml/sec
- Average flow rate – Should be around 10ml/sec
- Post Voided Residue (PVR) – Should be minimal
- The graph should be Bell pattern or Flat box type
Abnormal Uroflowmetry –
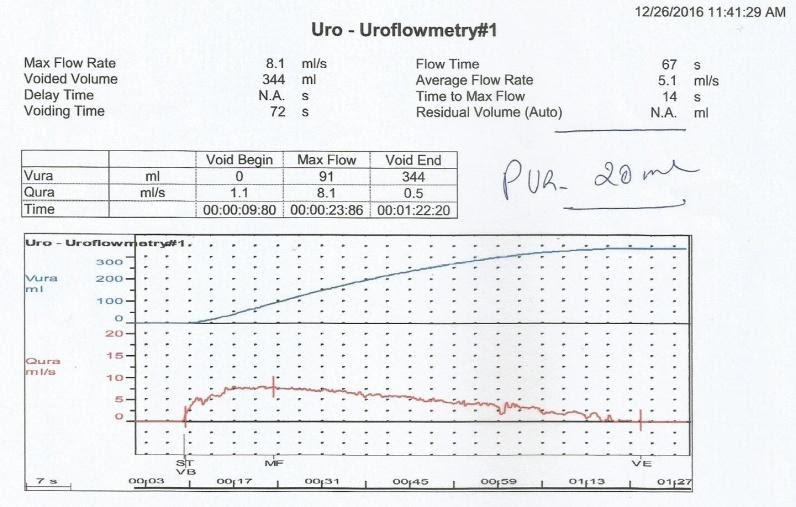
Normal Uroflowmetry –
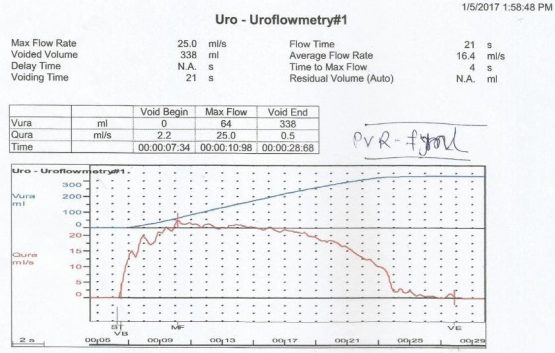
4. Retrograde / Ascending Urethrogram (RGU/AUG):
A radiological investigation in which a radio-opaque dye is injected into the urethra and the x-ray snap is taken.
Male:

Female:
5. Micturating / Voiding Cystourethrogram (MCUG/VCUG):
A radiological investigation in which the bladder is filled with a radio-opaque dye using a small tube and x-ray snaps are taken while the patient passes urine.

6. Cysto-urethroscopy:
It is an endoscopic investigation in which a Cysto-Urethroscope is used to visualize urethra & bladder.

Conventional Treatment
Language: Hindi
Language: English
Urethral Dilatation

- In Urethral dilatation, either Metal or Teflon dilators of different size are introduced into urethra under anesthesia.
- Dilators are introduced starting with a smaller size & then larger size
- Also called as serial dilatation or birthday dilatation
Balloon dilatation

- The procedure of dilatation of urethra using a Balloon catheter.
- It is done either under local anesthesia or under short general anesthesia.
Urethrotomy VIU / DVIU

- In this under anesthesia a cysto-urethroscope is introduced into the urethra, the fibrotic scar tissue is cut open to release the stricture.
- Different techniques are used including simple blade i. e. urotome, cold knife, and different lasers such as Holmium and Thulium laser.
Urethroplasty
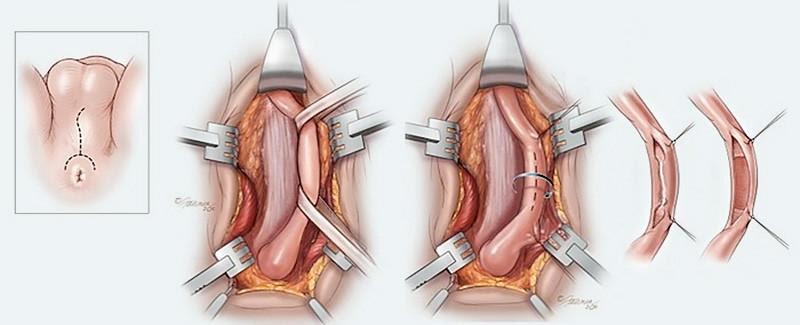
Urethroplasty is supposed to be the last resort for the management of urethral stricture. It is major open surgery. There are different types of urethroplasty. For short segment strictures, that much part of the urethra is excised and the two openings are joined together, this is called Anastomosis urethroplasty. For long or linear strictures, urethroplasty is performed in different ways. The commonest is Buccal Mucosal Graft Reconstructive Urethroplasty. In this, the constricted part of the urethra is excised and the buccal mucosa is used to reconstruct it. Unfortunately, stricture recurs even after urethroplasty and the patient has to involve in the same circle of VIU, dilatation & clean intermittent self-catheterization.
Self Catheterization / Self Dilatation / Clean Intermittent Self Catheterization (CISC)


- Patients are taught to introduce catheter into urethra on their own using an anesthetic gel
- This is done to maintain the caliber of urethra
- Usually advised after urethral dilatation, VIU & Urethroplasty
- Caliber of urethra reduces even after regular self catheterization & stricture recurs
- Certain complications are involved with self catheterization –
-
- Recurrent UTI
- Injury
- Rupture urethra
- New scar formation
- Multiple strictures
- False Passage
-
WE ALSO TREAT
BPH & Post TURP Status
Prostate gland enlarges & compresses the urethra
Bladder Outlet / Neck Obstruction
(BOO / BNO)
Blockage at the base or neck of the bladder
Interstitial Cystitis
Chronic condition causing bladder pressure with a persistent urge
Recurrent UTI & MDR UTI
A burning issue of the modern era
Hypotonic Bladder
A condition in which the bladder wall muscle tone reduces
Neurogenic bladder
Altered bladder function due to defects in the pathway of the micturition reflex
Incontinence
Inability to hold urine due to loss of voluntary control over the urinary sphincters
Enuresis – Bedwetting
Persistence of involuntary passage of urine even after the age of 5 years













